Are you struggling with unexplained fatigue, mood swings, or physical changes that seem beyond your control? If so, you’re not alone. Millions of people worldwide experience hormonal imbalances that significantly impact their quality of life. Hormone therapy offers a scientifically backed approach to restoring balance, libido, energy levels, mood, sleep quality, and overall vitality but is often overlooked despite its efficacy.
This comprehensive guide explores hormone therapy in depth, covering everything from what it is and how it works to the benefits, risks, and treatment options available. Whether you’re experiencing menopausal symptoms, low testosterone, considering hormone therapy, or simply want to understand how hormones affect your health, this article will provide the insights you need to make informed decisions about your well-being. We’ll discuss safety considerations and help you determine if hormone therapy might be the right choice for your unique situation.
Quick Takeaways
- Hormone therapy can effectively treat symptoms of hormonal imbalance, including hot flashes, night sweats, and mood changes that affect daily life.
- Both estrogen therapy and combined hormone therapy options exist, with treatment plans customized based on individual health history and needs..
- Bioidentical hormones are chemically identical to hormones your body produces naturally, offering an alternative to synthetic options
- Risks such as breast cancer, blood clots, and heart disease are generally low, but vary based on age, timing of treatment initiation, and individual risk factors.
- Hormone therapy for men addresses testosterone deficiency, while hormone therapy for women primarily focuses on estrogen and progesterone replacement.
- Cancer hormone therapy uses hormones or hormone-blocking drugs to slow or stop cancer growth in hormone-sensitive cancers.
- Working with healthcare professionals ensures proper monitoring, dosage adjustment, and ongoing safety assessment throughout treatment.
What Is Hormone Therapy?

Hormone therapy is a medical treatment that supplements or replaces hormones when your body doesn’t produce adequate amounts naturally. Think of hormones as chemical messengers that travel through your bloodstream, telling your organs and tissues what to do. When these messengers go silent or send mixed signals, your body struggles to function optimally.
The concept behind hormone therapy is straightforward: restore what’s missing or in decline to restore your hormonal balance. Your endocrine (chemical messaging) system produces hormones like estrogen, progesterone, testosterone, and thyroid hormones that regulate everything from metabolism and mood to sexual function, weight loss, and bone density. When your production declines due to aging, medical conditions, or surgical procedures, hormone therapy steps in to bridge the gap.
Understanding Hormone Balance Treatment
Hormone balance treatment goes beyond simple replacement. It involves comprehensive evaluation, precise dosing, and ongoing monitoring to ensure your hormone levels remain within optimal ranges. Primary care professionals assess multiple factors, including:
- Blood tests
- Symptom severity
- Medical history
- Lifestyle factors
The goal isn’t just to eliminate symptoms but to restore the delicate balance that allows your body to function at its best. This might involve adjusting multiple hormones simultaneously, as they often work together in complex feedback loops. For example, estrogen levels affect thyroid function, which in turn influences metabolism and energy levels.
Comparing Different Hormone Therapies
Here you can see all of the hormone therapies covered in the article at a glance, including delivery methods and who they are best suited for. At Azona Health, we offer estrogen for women and testosterone test kits in our shop, as well as a personalized patient portal to track your hormone recovery progress.
| Treatment Type | Delivery Method | Best For | Key Considerations |
| Estrogen-only therapy | Oral, patch, gel, ring | Women without a uterus | No endometrial cancer risk |
| Combined HRT | Oral, patch | Women with a uterus | Requires progestin protection |
| Local estrogen therapy | Vaginal cream, tablet, ring | Vaginal symptoms only | Minimal systemic absorption |
| Testosterone therapy | Injection, gel, patch | Men with low testosterone | Requires prostate monitoring |
| Cancer hormone therapy | Oral, injection | Hormone-sensitive cancers | Blocks rather than replaces hormones |
Hormone Therapy for Women

Women experience dramatic shifts in their female hormones throughout their lives, with menopause representing one of the most significant transitions. According to the National Institutes of Health (NIH) in 2023, approximately 1.3 million women in the United States become menopausal every year. Menopausal hormone therapy has evolved significantly over the past two decades, with providers now taking a more personalized approach based on individual risk factors, symptoms, and health goals.
Hormone therapy for women primarily addresses menopause symptoms that occur when the ovaries stop producing estrogen and progesterone during perimenopause (early menopause) and menopause. These menopausal symptoms can be debilitating. An estimated 75% of menopausal women are affected by hot flashes, with some experiencing them multiple times per hour. Night sweats can disrupt sleep, leading to fatigue, irritability, and difficulty concentrating. Vaginal dryness can make intimate relationships uncomfortable or painful. Beyond these immediate concerns, declining estrogen increases risks for osteoporosis and cardiovascular disease.
Types of Hormone Therapy
Several hormone therapy options exist to treat menopause symptoms, each with distinct characteristics:
- Estrogen-only therapy works for women who’ve had hysterectomies and don’t need endometrial protection from progestin.
- Combined HRT includes both estrogen and progestin for women with intact uteruses, available as cyclic therapy or continuous combined HRT.
- Local estrogen therapy delivers low-dose estrogen directly to vaginal tissues for symptoms like vaginal dryness without systemic absorption.
- A recent comparison published in Health Technology Review found that transdermal estrogen patches or gels may carry lower blood clot risks compared to oral hormone therapy
What Hormone Therapies are Most Effective for Women?
Studies show that estrogen therapy remains the most effective treatment for vasomotor symptoms like hot flashes and night sweats. For women who still have their uterus, combined hormone therapy that includes progestin (synthetic progesterone) protects against uterine cancer, also known as endometrial cancer, which excessive estrogen alone can increase your risk of.
Bioidentical Hormones vs Synthetic Options for Women
The debate between bioidentical hormones and synthetic hormones can be confusing for some looking into hormone treatment. Bioidentical hormones are called bioidentical because their molecular structure matches that of the hormones your body produces naturally, while synthetic hormones are ones that have a different chemical structure but serve the same role.
Hormone Therapy for Men

While discussions often focus on women’s hormone therapy, men experience their own hormonal changes that can benefit from treatment. Male hormone production declines gradually, with serum testosterone levels dropping approximately 0.4% annually for men 40-70 years old, with free testosterone declining more than 1% per year. This gradual decline, sometimes called andropause (male menopause) or late-onset hypogonadism, affects energy, muscle mass, bone density, sexual function, and mood.
Doctors may prescribe testosterone replacement therapy when blood tests confirm low testosterone levels and symptoms significantly impact quality of life. Symptoms include persistent fatigue, reduced libido, erectile dysfunction, depression, difficulty concentrating, and loss of muscle mass despite exercise.
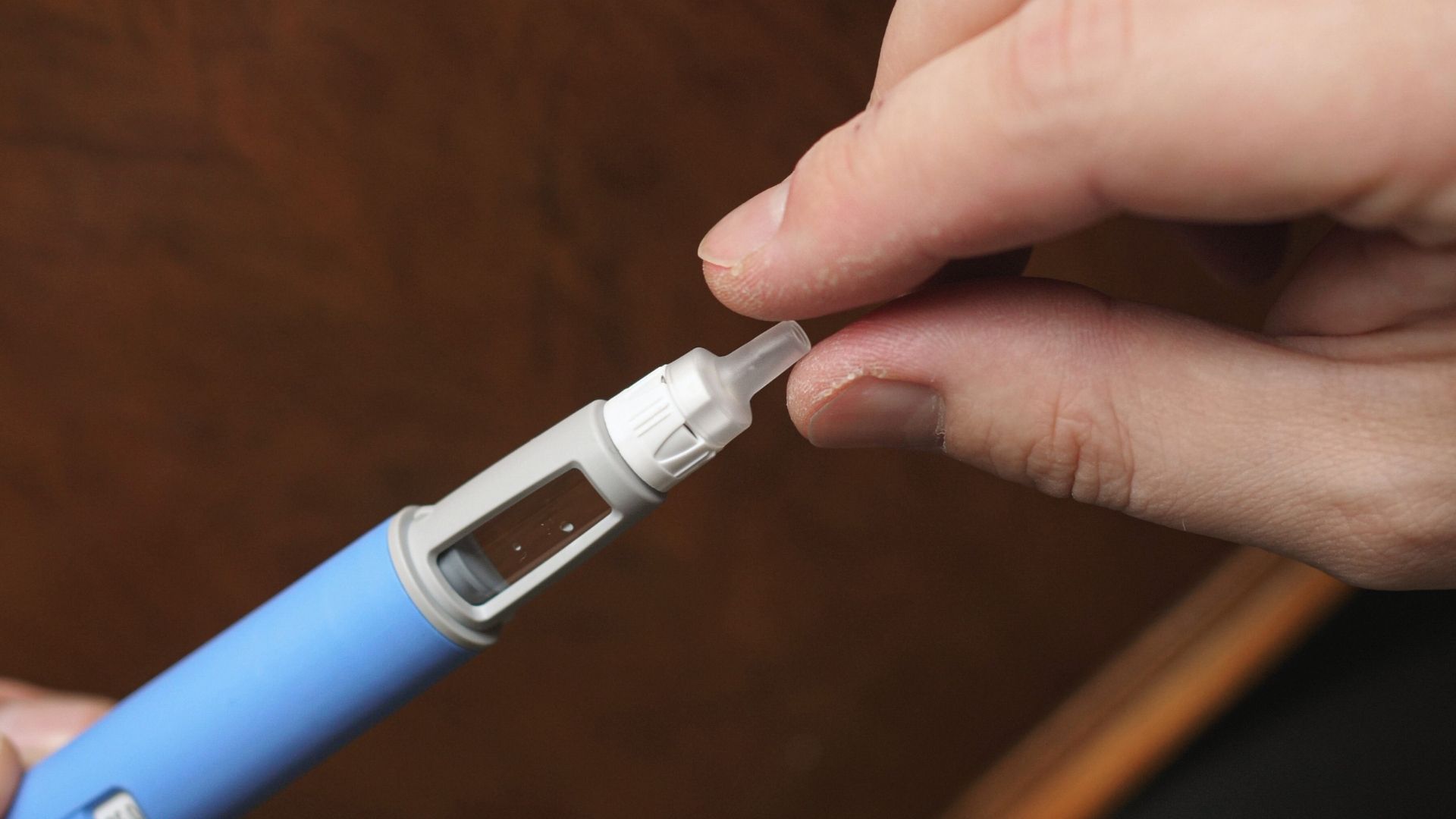
Testosterone therapy comes in multiple forms: injections, topical gels, patches, nasal sprays, and pellets implanted under the skin. Each delivery method has advantages and disadvantages regarding convenience, cost, and how consistently it maintains testosterone levels.
Hormone Therapy for Cancer Treatment
Cancer hormone therapy represents a completely different application of hormones in medicine. Rather than replacing deficient hormones, cancer hormone therapy blocks or removes hormones that fuel certain cancers. This systemic therapy is called hormonal therapy or endocrine therapy when used for cancer treatment.
Hormone Therapy for Breast Cancer
Breast cancers that test positive for estrogen or progesterone receptors grow in response to these hormones. It is estimated that 70%-80% of breast cancers are hormone receptor-positive. For these breast cancers, blocking hormones can significantly reduce recurrence risk and improve survival.
Prostate Cancer Hormone Therapy
Prostate cancer cells often depend on testosterone and other male hormones to grow. Androgen deprivation therapy (ADT) treats cancer by lowering testosterone levels or blocking testosterone from reaching cancer cells. This represents a key treatment for advanced prostate cancer and is sometimes used alongside radiation therapy for localized disease.
Benefits of Hormone Therapy
When used appropriately, hormone therapy offers substantial benefits that extend beyond symptom relief. Understanding these advantages helps you weigh potential benefits against risks.
For menopausal symptoms, hormone therapy provides unmatched effectiveness. No other treatment comes close to reducing hot flashes and night sweats as effectively. This improvement in vasomotor symptoms translates to better sleep quality, improved mood, enhanced cognitive function, and better overall quality of life.
Estrogen therapy significantly reduces bone loss and fracture risk. Postmenopausal women lose bone density rapidly without estrogen’s protective effects. Studies show hormone therapy reduces hip fractures by 30-40%and vertebral fractures by similar amounts. For women at high osteoporosis risk, this benefit alone may justify hormone therapy use.
Systemic hormone therapy also preserves vaginal and urinary tract health. Estrogen maintains vaginal tissue thickness, elasticity, and natural lubrication. It reduces urinary tract infection frequency and may improve some types of urinary incontinence. These effects improve sexual function and comfort.
Risks and Side Effects of Hormone Therapy
No medical treatment comes without potential downsides, and hormone therapy is no exception. Understanding these risks allows you to make informed decisions and recognize concerning symptoms early.
Breast Cancer Risk
The connection between hormone therapy and breast cancer risk generates the most concern and confusion among those looking into hormone therapy. Here’s what scientific evidence actually says:
Estrogen-only therapy for women who’ve had hysterectomies doesn’t appear to increase the risk of breast cancer. A 2023 long-term meta-analysis taking into account the 2002 trials by the Women’s Health Initiative found no increased breast cancer risk; in fact, it found that estrogen therapy may even reduce breast cancer incidence and mortality.
The study did find that combined hormone therapy that includes progestin does increase breast cancer risk, but the absolute risk remains small. Taking combined HRT for five years increases breast cancer risk by approximately 1-3 cases per 1,000 women per year. For perspective, obesity, alcohol consumption, and lack of exercise carry similar or greater breast cancer risks.
Blood Clots and Stroke
Hormone therapy increases blood clot risk, particularly with oral estrogen formulations. Blood clots can occur in leg veins (deep vein thrombosis) or travel to the lungs (pulmonary embolism). However, the absolute risk with treatment remains low. Transdermal estrogen delivered through patches or gels appears to carry a lower blood clot risk than oral estrogen. This difference occurs because transdermal estrogen bypasses the liver, avoiding the increase in clotting factors that oral estrogen triggers.
Stroke risk also increases slightly with hormone therapy, particularly in older women. This reinforces the importance of starting hormone therapy during the menopausal transition rather than years later.
Cardiovascular Health Considerations
The relationship between hormone therapy and heart disease is complex and depends on when treatment begins. When started within 10 years of menopause (before age 60 on average), hormone therapy may reduce cardiovascular disease risk. This timing-dependent effect explains why earlier studies showed increased heart disease risk; they included many older women starting therapy years after menopause.
For younger women transitioning through early menopause, either naturally or surgically, hormone therapy appears to protect cardiovascular health. The loss of estrogen’s protective effects at a young age significantly increases heart disease risk, and hormone therapy may counteract this.
Other Potential Risks
Additional concerns include:
- Endometrial cancer risk increases dramatically with estrogen-only therapy in women who still have a uterus, which is why progestin is added for protection.
- Ovarian cancer risk may increase slightly with long-term hormone therapy use, though evidence remains inconsistent.
- Gallbladder disease and liver disease risks increase with oral estrogen.
- Side effects like breast tenderness, bloating, headaches, and mood changes affect some women, though often improve with dose adjustment/
Is Hormone Replacement Therapy Safe?
Generally, yes, though safety in hormone replacement depends on multiple factors, including your age, time since menopause, medical history, family history, and the specific type and dose of hormone therapy.
For women under 60 or within 10 years of menopause experiencing bothersome symptoms, hormone therapy generally carries more benefits than risks. The key is appropriate patient selection and the use of the lowest effective dose for the shortest duration needed.
Healthcare professionals now take a personalized approach, carefully weighing individual risk factors. Women with a history of breast cancer, blood clots, stroke, heart disease, or liver disease typically shouldn’t use systemic hormone therapy. Those at high risk for these conditions need extra caution.
Regular monitoring ensures ongoing safety. Your doctor should schedule follow-up visits to assess symptom control, side effects, and whether continuing treatment remains appropriate. Many women use hormone therapy for several years during the most symptomatic period, then gradually taper off.
Natural Hormone Replacement Therapy
Many people seek natural hormone replacement therapy alternatives, hoping to avoid pharmaceutical interventions. Several approaches fall under this umbrella, with varying degrees of effectiveness and scientific support.
Lifestyle modifications provide a foundation for hormonal health. Regular exercise, particularly strength training, supports healthy hormone production and reduces menopausal symptoms. A diet rich in phytoestrogens from soy, flaxseeds, and legumes may modestly reduce hot flashes in some women. Stress reduction through meditation, yoga, or other practices helps regulate cortisol and other stress hormones that can disrupt overall hormone balance.
Herbal supplements like black cohosh, red clover, and dong quai are marketed for menopausal symptoms. However, scientific evidence for their effectiveness remains mixed. Also, these supplements aren’t completely risk-free; they can interact with medications and may cause side effects. The lack of regulation means quality and potency vary significantly between products.
Treatment Options and Delivery Methods

Hormone replacement options have expanded significantly, allowing for personalized treatment approaches. Understanding available delivery methods helps you discuss preferences with your healthcare provider.
Systemic Estrogen Delivery
Systemic estrogen therapy treats symptoms throughout your body:
- Oral tablets remain the most prescribed form, taken daily, but carry a higher blood clot risk due to liver metabolism
- Transdermal patches applied to the skin twice weekly release steady estrogen amounts and may be safer for cardiovascular health
- Estrogen gels rubbed on arms or thighs daily offer flexibility in dosing
- Vaginal rings inserted every three months release systemic-dose estrogen continuously
- Injections and pellets provide longer-lasting options, though with less dosing flexibility
Local Estrogen Therapy
Local estrogen therapy delivers low doses directly to vaginal tissue. These treatments effectively relieve vaginal symptoms and vaginal dryness without significantly raising blood estrogen levels. Options include:
- Vaginal creams
- Tablets
- Low-dose rings
Women with contraindications to systemic therapy can often safely use local estrogen.
Progestin Options
Women with a uterus need progestin to protect against endometrial cancer when taking estrogen. Progestin can be taken as oral pills, combined with estrogen in a single pill, delivered through progesterone-releasing intrauterine devices, or included in combination patches.
Cyclic therapy involves taking progestin for part of each month, mimicking natural menstrual cycles and causing monthly bleeding. Continuous combined HRT takes both hormones daily without breaks, typically stopping periods after several months.
Working with Healthcare Professionals for Hormone Replacement Therapy (HRT)
Navigating hormone therapy requires partnership with knowledgeable healthcare professionals who understand both the science and your individual circumstances. Finding the right provider makes a significant difference in your treatment experience and outcomes.
Start by discussing your symptoms in detail. Don’t minimize or dismiss what you’re experiencing and describe how symptoms affect your daily life, work, relationships, and overall wellbeing. This information helps your doctor assess whether hormone therapy is appropriate and what treatment goals matter most to you.
Your medical history matters enormously. Be thorough and honest about personal and family history of breast cancer, heart disease, blood clots, stroke, and other conditions. This information guides treatment decisions and risk assessment. Bring a list of current medications and supplements, as interactions can occur.
Expect comprehensive evaluation before starting hormone therapy. Your doctor should order blood tests to assess hormone levels, perform a physical exam including breast and pelvic exams, review your latest mammogram results, and discuss your individual risk factors. Some doctors also check cholesterol, blood sugar, and liver function.
Treatment planning should be collaborative. Discuss your preferences regarding delivery methods, dosing schedules, and treatment goals. Ask about alternatives if you have concerns about certain approaches. Understand that finding the right dose and formulation may take several months of adjustment.
Frequently Asked Questions About Hormone Therapy
What does hormone therapy do?
Hormone therapy supplements or replaces hormones your body no longer produces in adequate amounts. It can relieve symptoms like hot flashes, night sweats, mood changes, and fatigue caused by hormonal imbalances. The treatment restores optimal hormone levels, improving energy, sleep quality, bone density, and overall well-being. For cancer patients, hormone therapy blocks hormones that fuel tumor growth.
What are the disadvantages of hormone therapy?
Hormone therapy carries potential risks, including increased breast cancer risk with some forms of long-term use, blood clots, stroke, and heart disease, particularly when started later in life. Side effects may include bloating, breast tenderness, headaches, and mood changes. Certain medical conditions, like previous blood clots or liver disease, make hormone therapy unsuitable for some individuals.
What are the two types of hormone therapy for women?
The two main types are estrogen-only therapy and combined hormone therapy. Estrogen-only therapy is for women who’ve had hysterectomies. Combined hormone therapy includes both estrogen and progestin, protecting the uterus from cancer in women who still have one. Additionally, local hormone therapy treats vaginal symptoms specifically without systemic effects.
What is the procedure for hormonal therapy?
Hormonal therapy starts with a comprehensive evaluation, including blood tests and a medical history review. Your doctor prescribes appropriate hormones delivered through pills, patches, gels, or injections. Regular follow-up visits monitor symptom improvement, adjust dosages as needed, and check for potential side effects, ensuring safe and effective treatment.
What is done in hormone therapy?
Hormone therapy replaces deficient hormones through medications delivered as pills, patches, gels, creams, or injections. Treatment restores estrogen, progesterone, or testosterone levels to alleviate symptoms like hot flashes, fatigue, and mood changes. Your healthcare provider monitors your response, adjusts dosages, and conducts regular health screenings to ensure the therapy remains safe and effective for your needs.
What are the negative effects of hormone therapy?
Negative effects of taking hormone therapy include increased risks of breast cancer, blood clots, stroke, and heart disease. Common side effects are bloating, breast tenderness, headaches, nausea, and mood swings. Some experience weight gain, vaginal bleeding, or gallbladder problems. Risks vary based on age, health history, dosage, and treatment duration, requiring managed medical supervision.
Choosing Hormone Therapy with Azona Health
Hormone therapy represents a powerful tool for managing symptoms and health concerns related to hormonal imbalances, but it’s not a one-size-fits-all solution. As we’ve explored, hormone replacement therapy offers significant benefits for many people experiencing menopausal symptoms, helping to relieve hot flashes, preserve bone density, and improve quality of life. At the same time, understanding the risks, including increased breast cancer risk with combined therapy, blood clots, and cardiovascular considerations, is essential for making informed choices.
Ready to reclaim your vitality? Azona Health specializes in the best personalized hormone replacement therapy tailored to your unique needs through our innovative telehealth services. Our experienced team provides comprehensive evaluation, ongoing monitoring, and compassionate care to help you feel like yourself again. Get started today and take the first step toward hormonal balance and renewed energy.